Osteoporosis is a chronic condition affecting bone density and strength, increasing the risk of fractures. Often referred to as a “silent disease,” osteoporosis develops gradually and is frequently undiagnosed until a fracture occurs. In this article, we will delve into the causes, symptoms, risk factors, and management strategies to provide a detailed understanding of osteoporosis and how to address it effectively.
What Is Osteoporosis?
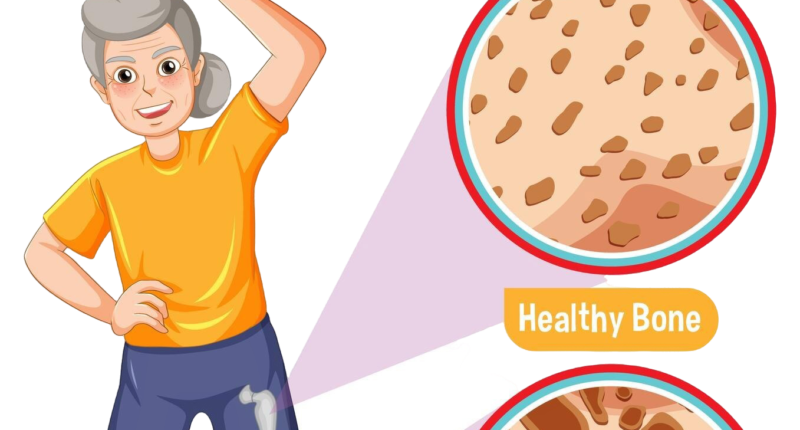
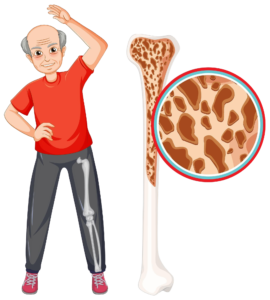
Osteoporosis, meaning “porous bones,” is a condition where bone mineral density (BMD) is significantly reduced. This makes bones fragile and more susceptible to fractures, even with minor falls or injuries. The most commonly affected areas are the hips, spine, and wrists, although any bone in the body can be impacted.
Symptoms of Osteoporosis
Osteoporosis is often asymptomatic in its early stages. However, as the condition progresses, the following symptoms may appear:
- Chronic back pain: Caused by fractured or collapsed vertebrae.
- Loss of height: A gradual decrease in height due to spinal compression.
- Stooped posture: A noticeable curvature in the upper back, known as kyphosis.
- Frequent fractures: Especially in the hips, wrists, or spine, after minimal trauma.
Causes of Osteoporosis
Bone is a dynamic tissue, constantly undergoing remodelling, where old bone is replaced by new bone. Osteoporosis occurs when this balance is disrupted, leading to greater bone resorption than formation. Key causes include:
- Age: Bone density naturally decreases with age.
- Hormonal changes: Estrogen decline in women post-menopause and testosterone reduction in men can accelerate bone loss.
- Genetic factors: A family history of osteoporosis increases the risk.
- Lifestyle choices: Sedentary lifestyles, poor nutrition, and smoking contribute to weakened bones.
Risk Factors for Osteoporosis
Understanding the risk factors is crucial for early intervention. The main risk factors include:
- Gender: Women are at higher risk than men.
- Age: Older adults, particularly those over 50, are more susceptible.
- Ethnicity: Caucasians and Asians are more prone to osteoporosis.
- Family history: A family history of fractures or osteoporosis increases vulnerability.
- Dietary deficiencies: Low calcium and vitamin D intake can weaken bones.
- Medical conditions: Disorders like rheumatoid arthritis, hyperthyroidism, and celiac disease elevate risk.
- Medications: Long-term corticosteroids or certain anti-seizure drugs can reduce bone density.
How Is Osteoporosis Diagnosed?
Early detection is critical for managing osteoporosis effectively. Diagnosis typically involves:
- Bone Density Test (DXA Scan): A dual-energy X-ray absorptiometry (DXA) scan measures bone density at specific sites, such as the hip and spine.
- Blood Tests: To rule out other medical conditions and evaluate calcium and vitamin D levels.
- Fracture Risk Assessment Tool (FRAX): A tool to estimate the risk of fractures over the next 10 years.
Preventing Osteoporosis
Prevention begins with adopting a bone-friendly lifestyle early in life. Key strategies include:
- Nutrition for Strong Bones
- Calcium: Adults require 1,000–1,200 mg of calcium daily. Include dairy products, leafy greens, and fortified foods in your diet.
- Vitamin D: This nutrient aids calcium absorption. Spend time in sunlight and consume fatty fish, egg yolks, and fortified foods.
- Regular Exercise
- Weight-bearing exercises: Walking, dancing, and hiking promote bone health.
- Resistance training: Strength training exercises improve bone density and muscle mass.
- Lifestyle Modifications
- Quit smoking and limit alcohol consumption, as both negatively impact bone health.
- Maintain a healthy body weight to reduce strain on bones.
Treatment Options for Osteoporosis
While osteoporosis cannot be entirely reversed, effective treatments can manage symptoms and reduce fracture risks. Options include:
- Medications
- Bisphosphonates: Slow down bone resorption and increase bone density.
- Selective Estrogen Receptor Modulators (SERMs): Mimic estrogen’s protective effects on bone.
- Parathyroid hormone-related treatments: Stimulate bone growth.
- Calcium and Vitamin D Supplements: Essential for bone strength.
- Physical Therapy
Supervised physical therapy helps improve balance, posture, and muscle strength, reducing fall risks.
- Surgical Interventions
For severe spinal fractures, procedures like vertebroplasty or kyphoplasty may stabilize the spine and alleviate pain.
Living with Osteoporosis
Managing osteoporosis requires a holistic approach. Incorporate these habits into your daily routine:
- Use assistive devices, like grab bars and anti-slip mats, to prevent falls.
- Schedule regular medical check-ups to monitor bone health.
- Stay active with tailored exercises to maintain mobility and strength.
Future Trends in Osteoporosis Management
Advances in osteoporosis research are paving the way for improved treatments. Emerging therapies, such as biological agents targeting bone remodelling pathways, hold promise for more effective management of this condition. Genetic testing and personalized medicine may also revolutionize prevention strategies.
Osteoporosis is a manageable condition with early detection and lifestyle adjustments. By focusing on prevention, adopting healthy habits, and seeking medical advice when necessary, individuals can maintain strong bones and reduce the risk of fractures.