Developing and delivering new drugs to market is a critical endeavour in modern medicine. It combines scientific innovation, rigorous testing, regulatory scrutiny, and often, an urgent need to address pressing health crises. While the goal is to save lives and improve quality of life, the race to develop and approve drugs brings both opportunities and challenges.
This article explores the intricate journey of drug development, the factors accelerating the process, and the delicate balance between speed and safety.
Understanding the Drug Development Process
Bringing a new drug to market involves several key stages, each designed to ensure efficacy, safety, and quality:
1. Discovery and Preclinical Research
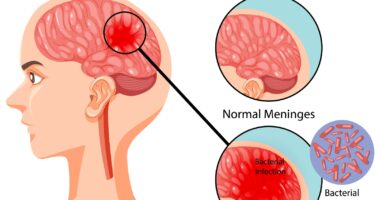
- Drug Discovery: Researchers identify potential drug compounds by studying disease mechanisms and screening thousands of molecules.
- Preclinical Testing: Before human trials, compounds undergo laboratory and animal testing to assess safety and efficacy.
2. Clinical Trials
Clinical trials occur in three phases, each with increasing participant numbers and complexity:
- Phase I: Focuses on safety and dosage in a small group of healthy volunteers.
- Phase II: Test the drug’s effectiveness in a larger group of patients.
- Phase III: Involves thousands of participants to confirm effectiveness, monitor side effects, and compare the drug to existing treatments.
3. Regulatory Review
Regulatory agencies, such as the U.S. Food and Drug Administration (FDA) or the European Medicines Agency (EMA), evaluate trial data to approve or deny drug applications.
4. Post-Market Surveillance
Even after approval, drugs are monitored for long-term safety and effectiveness in the broader population.
The Push to Accelerate Drug Approval
Recent global health crises, such as the COVID-19 pandemic, have underscored the need to expedite drug approvals. Innovations and strategies driving faster market access include:
1. Breakthrough Therapies
Regulatory bodies offer designations like “Breakthrough Therapy” to drugs showing early promise in treating serious conditions. This allows for accelerated review and development timelines.
2. Adaptive Clinical Trials
Innovative trial designs, such as adaptive trials, enable modifications based on interim results, reducing time and cost.
3. Emergency Use Authorizations (EUA)
In emergencies, agencies may grant EUA to drugs and vaccines before full approval, as with COVID-19 vaccines.
4. Artificial Intelligence (AI) in Drug Discovery
AI accelerates drug discovery by analyzing vast datasets to identify promising compounds more quickly than traditional methods.
Balancing Speed and Safety
While expediting drug approvals is vital during crises, it must not come at the expense of safety. History has shown the dangers of rushing without adequate testing:
- Thalidomide Tragedy (1960s): Prescribed for morning sickness, thalidomide caused birth defects, highlighting the importance of rigorous safety evaluations.
- Vioxx Recall (2004): This arthritis drug was withdrawn after being linked to cardiovascular risks, emphasizing the need for long-term monitoring.
Regulators must strike a balance between urgency and caution to protect public health while addressing unmet medical needs.
The Impact of Accelerated Drug Approvals
1. Improved Patient Outcomes
Faster drug approvals can save lives by providing earlier access to treatments for conditions like cancer, rare diseases, and infectious outbreaks.
2. Economic Benefits
Successful drugs contribute to the pharmaceutical industry’s growth, job creation, and economic development.
3. Ethical Considerations
Expediting drug development raises ethical questions about trial design, participant safety, and equitable access. Ensuring that vulnerable populations are not disproportionately affected is critical.
Challenges in the Race to Market
1. High Costs and Risks
Developing a single drug can take 10–15 years and cost billions of dollars, with no guarantee of success.
2. Regulatory Hurdles
Meeting the stringent requirements of regulatory agencies is a complex and time-intensive process.
3. Drug Accessibility
Once approved, drugs must be affordable and widely available to maximize public health impact.
Conclusion
The race to get drugs to market is a complex interplay of innovation, regulation, and ethical responsibility. While the need for speed is undeniable, ensuring the safety, efficacy, and accessibility of new treatments remains paramount. By leveraging technology, fostering collaboration, and maintaining rigorous oversight, we can navigate the challenges and deliver life-saving drugs to those who need them most.